April is Testicular Cancer Awareness Month.
This podcast on
Testicular Cancer and Fertility Preservation,
presented by Dr. Landon Trost
of the Mayo Clinic’s Urology Dept.,
provides some valuable information.Download
What Is Testicular Tissue Freezing?
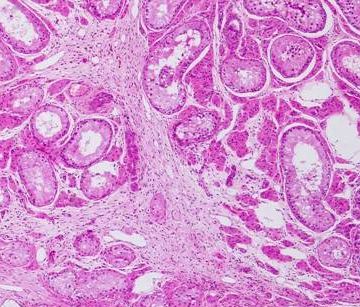
Sperm banking is not an option for pre-pubescent boys who are not yet producing sperm. However, these boys do have stem cells in their testes that are poised to begin producing sperm at puberty. There are experimental studies underway to preserve testicular tissue obtained by biopsy and freeze it for future use. The tissue contains stem cells which will be able to start spermatogenesis (sperm production). Testicular tissue freezing is considered experimental and is generally only offered in a research setting with IRB oversight. Several studies are developing protocols that will enable scientists and physicians to use the frozen/thawed testicular tissue and stem cells to produce sperm in the laboratory or by re-implanting, years later, back into the individual. Research has proven these strategies are effective in animals and it is envisioned that they will also be effective in humans.
Who Uses Testicular Tissue Freezing and Storage and Why?
Pre-pubescent boys who have cancer or other diseases that may interfere with or destroy sperm production use testicular tissue freezing to protect their fertility. The tissue is put into long term storage. Several fertility centers in the U.S. and abroad are processing and freezing testicular tissue in anticipation that new stem cell-based therapies will be available in the future to help these patients achieve pregnancy and have their own biological children.
How Do I Get Started With Testicular Tissue Storage?
The Fertility Preservation Program of Pittsburgh at the University of Pittsburgh Medical Center (UPMC) has established a dedicated phone line (412-641-7475) and email address [email protected] that patients and their physicians may use to learn about the reproductive side effects of their treatments and options for preserving their fertility. This is a discussion that must take place before toxic therapies are initiated and fertility is irreversibly destroyed. There are no standard options to preserve the fertility of boys who are not yet producing sperm. For these young patients, The Fertility Preservation Program of Pittsburgh is approved to freeze testicular tissue that might be used in the future to restore fertility when experimental techniques emerge from the research pipeline. This experimental procedure is currently offered at the Children’s Hospital of Pittsburgh of UPMC, the Ann and Robert Lurie Children’s Hospital of Chicago, the Children’s Hospital of Orange County, the Children’s national Medical Center in Washington DC, and Mayo Clinic in Rochester, MN. Additional sites are preparing to participate in this multi-center study. For more information on standard and experimental options for preserving fertility please visit http://fertilitypreservationpittsburgh.org, email [email protected] or call (412-641-7475). The Fertility Preservation Program of Pittsburgh is a multidisciplinary working group that includes key stake holders at Magee-Womens Research Institute, Magee-Womens Hospital of UPMC and Children’s Hospital of Pittsburgh of UPMC.
The Future of Testicular Tissue Storage
A small portion (~25%) of the biopsy from each patient will be donated to research. This is necessary to allow research to happen and to develop the best methods to freeze, thaw, and use the testicular tissue. Experimental options that may be available in the future for patients who preserve testicular tissue are transplantation of spermatogonial stem cells (SSC) back into the testes of the patient; maturation of spermatozoa in testicular tissue organ culture and testicular tissue autografting or xenografting. It is important to note that except for SSC transplantation, all of these methods will require the use of IVF/ICSI to achieve fertilization and pregnancy. All testicular tissue based fertility options are considered experimental and have not been fully translated to clinical practice.